Rectal cancer can be challenging to diagnose because the signs and symptoms are often subtle or not present in early stages. While rectal cancer has historically been more common in people over the age of 50, recent years have seen a concerning rise in cases among younger adults. Colorectal cancer is now the leading cause of cancer-related death in the US in men younger than age 50, and the second leading cause of cancer-related death in women younger than age 50. Recognizing the early signs and symptoms of rectal cancer is crucial for early diagnosis and effective treatment. Here, we’ll explore the key risk factors, common symptoms to watch for, the various stages of rectal cancer, and when to begin screening. Understanding these details can help save lives and improve health outcomes through early intervention.
What Is Rectal Cancer?
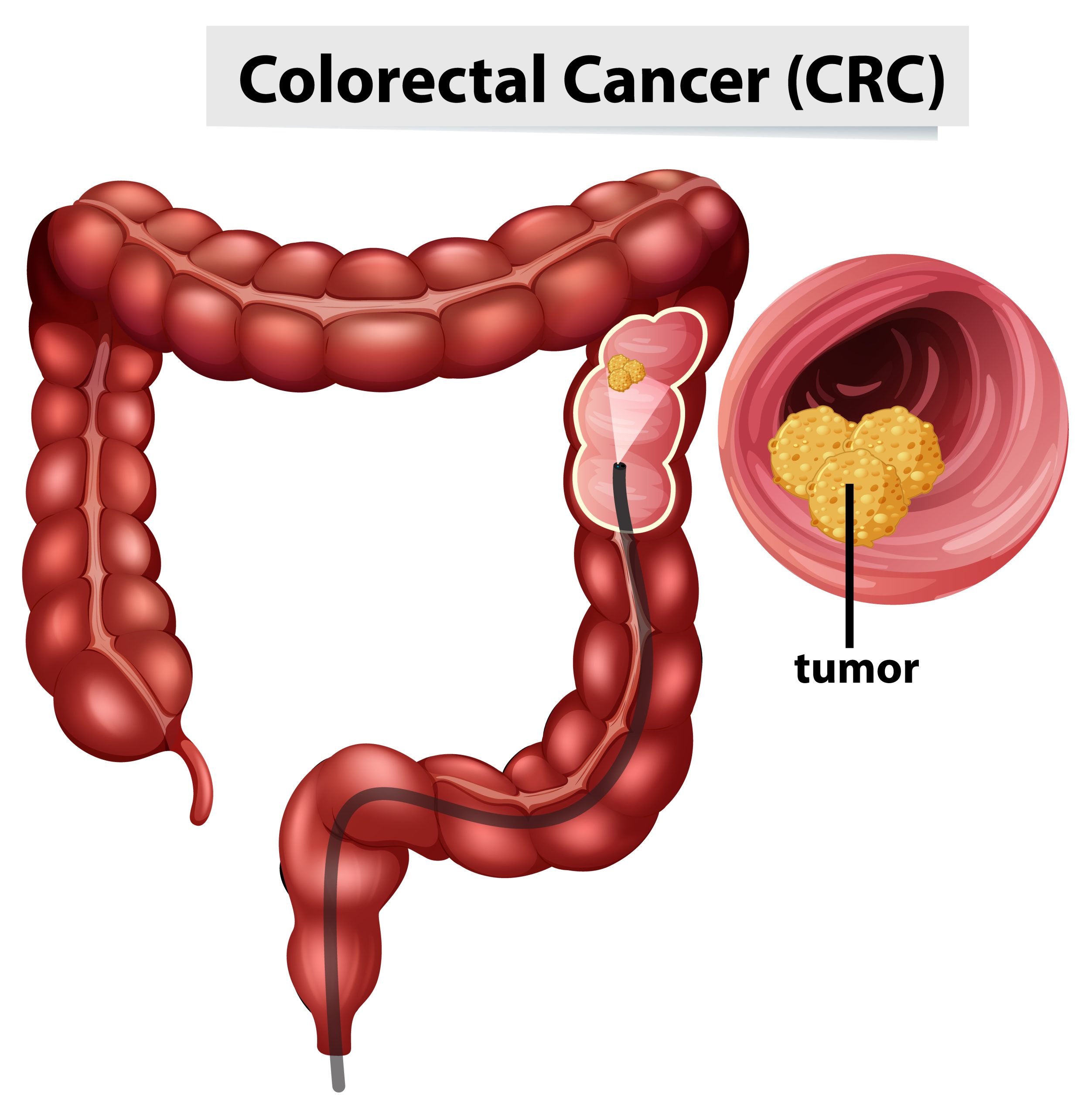
Rectal cancer is a type of colorectal cancer that begins as an abnormal growth of cells in the last several inches of the large intestine, known as the rectum. Rectal cancer develops when healthy cells in the rectum’s lining mutate and grow abnormally, leading to the formation of a mass or tumor. Over time, these cancer cells can invade nearby tissues and spread to other parts of the body, including the lymph nodes, liver, or lungs.
The rectum is part of the digestive tract that stores stool before it leaves the body. Because it’s so close to the colon, rectal and colon cancers are often grouped together and referred to as colorectal cancers. However, the treatment of these two cancers can differ due to the rectum’s location within the pelvis and its proximity to other organs.
Key Risk Factors for Rectal Cancer
Several factors can increase your risk of developing rectal cancer:
- Age: Most cases of rectal cancer are diagnosed after age 50, but in recent years, more people younger than 50 are being diagnosed.
- Family history: Having a parent, sibling, or child with colorectal cancer increases risk.
- Diet: High intake of red or processed meat and low fiber consumption can raise risk.
- Inflammatory bowel disease (IBD): Chronic inflammation from an IBD such as ulcerative colitis or Crohn’s disease can increase susceptibility.
- Lifestyle factors: Smoking, heavy alcohol consumption, obesity, and lack of exercise also contribute to the risk of developing rectal cancer.
- Genetics: Inherited syndromes like Lynch syndrome and familial adenomatous polyposis (FAP) dramatically increase lifetime risk.
Do Early Stages of Rectal Cancer Show Symptoms?
In its earliest stages, rectal cancer may not cause any noticeable symptoms. Many people are diagnosed during routine colorectal cancer screening, such as a colonoscopy, before symptoms appear. When signs do develop, they’re often subtle and can be mistaken for less serious conditions like hemorrhoids, irritable bowel syndrome (IBS), or an anal fissure.
Early detection is essential for better outcomes. When caught at an early stage — before the cancer has spread beyond the rectum — treatment success rates are high. This is why organizations like the American Cancer Society recommend starting screening at age 45 for people at average risk and earlier for those with a family history or other risk factors.
Top 10 Signs and Symptoms of Rectal Cancer
Rectal cancer can show up in various ways depending on the tumor’s location and progression. Here are the top 10 signs and symptoms to watch for:
- Rectal Bleeding: One of the most common warning signs. Bright red blood may appear on toilet paper, in the toilet bowl, or mixed with stool.
- Blood in the Stool: Stools may appear dark or tarry due to hidden (occult) bleeding higher up in the rectum or colon.
- Changes in Bowel Habits: You may notice persistent diarrhea, constipation, or a change in stool consistency lasting more than a few days.
- Feeling of Incomplete Bowel Movements: Also called tenesmus, this is the feeling that you still need to have a bowel movement even after going to the bathroom.
- Narrow or Ribbon-Like Stools: As tumors grow, they may narrow the space through which stool passes, causing long, thin stools.
- Unexplained Weight Loss: Cancer cells use up energy, and systemic inflammation can cause unintentional weight loss even when diet remains the same.
- Fatigue or Weakness: Chronic blood loss can lead to anemia, a decrease in red blood cells, resulting in tiredness, weakness, or pale skin.
- Abdominal Discomfort or Cramps: Persistent bloating, pain, or fullness in the abdomen can point to a digestive tract that isn’t functioning properly.
- Mucus in Stool: Tumors may cause excess mucus production, which sometimes appears in bowel movements.
- Rectal Pain or Pressure: Pain during bowel movements or a constant feeling of fullness in the rectum can indicate an advanced stage of the disease.
Not everyone experiences all these symptoms, and their severity doesn’t always reflect how advanced the cancer is, which highlights the importance of routine screening for rectal cancer.
Rectal Cancer Stages: Why Early Stage Screening Matters
Rectal cancer is staged based on how deeply the tumor has penetrated the rectal wall and whether it has spread to lymph nodes or distant organs.
| Stage 0 (Carcinoma in situ) | Abnormal cells are present but haven’t spread beyond the inner lining. |
| Stage I | Cancer has grown into the rectal wall but hasn’t reached lymph nodes. |
| Stage II | The tumor extends through the wall into nearby tissue but not to lymph nodes. |
| Stage III | Cancer has spread to nearby lymph nodes but not distant organs. |
| Stage IV | The cancer has metastasized to distant parts of the body, such as the liver or lungs. |
Early-stage rectal cancer (Stage 0–I) is often curable through surgery alone, while later stages may require chemotherapy and radiation. This makes routine screening essential for detecting precancerous polyps or early tumors before symptoms appear.
What Causes Symptoms to Worsen Over Time?
As rectal cancer grows, it can obstruct the passage of stool and invade nearby structures, worsening symptoms and affecting other body systems.
- Increased bleeding can lead to chronic anemia and fatigue.
- Tumor growth may block the rectum entirely, causing severe constipation or bowel obstruction.
- Cancer spread (metastasis) to the liver or lungs can lead to additional symptoms, such as jaundice, persistent cough, or bone pain.
Inflammation and immune response triggered by cancer cells also play a role. As the tumor grows, it releases substances that disrupt normal bowel function and affect metabolism throughout the body. Untreated rectal cancer can eventually cause systemic symptoms, including severe weight loss, loss of appetite, and generalized weakness.
Treatment Options for Rectal Cancer
Treatment for rectal cancer depends on the stage of the disease, overall health, and whether the cancer has spread. Current approaches often involve a combination of therapies to maximize success.
- Surgery – Surgery is often the first-line treatment for localized rectal cancer. Procedures may include:
- Local excision: Removal of small, early-stage tumors through the rectum.
- Low anterior resection (LAR): Removes the affected rectum section while preserving bowel continuity.
- Abdominoperineal resection (APR): Removes the rectum and anus; may require a permanent colostomy.
- Radiation Therapy – May be used before or after surgery, radiation helps shrink tumors, kill remaining cancer cells, and reduce recurrence risk.
- Chemotherapy – Medications that target and kill cancer cells throughout the body.
- Targeted Therapy and Immunotherapy – These advanced treatments use drugs that block specific molecules involved in cancer growth or boost the immune system’s ability to attack cancer cells.
- Palliative Care – For advanced cancer, palliative treatments focus on relieving symptoms, improving comfort, and maintaining quality of life.
Because rectal cancer treatment can impact bowel function, fertility, and daily living, multidisciplinary care involving oncologists, surgeons, and dietitians is essential for overall health.
When to See a Doctor About Rectal Cancer Symptoms
Early detection is the best defense against rectal cancer. Contact your healthcare provider if you have any concerns about rectal cancer or you experience any of the following:
- Persistent rectal bleeding or blood in the stool
- Unexplained changes in bowel habits lasting more than two weeks
- Ongoing abdominal discomfort, bloating, or cramping
- Unexplained fatigue or weight loss
- A family history of colorectal cancer or polyps
Doctors may perform blood tests, a digital rectal exam, colonoscopy, or imaging tests like CT scans to evaluate symptoms. Biopsies (tissue samples) are analyzed to confirm diagnosis and determine the cancer’s stage.
In the United States, colorectal cancer is the second leading cause of cancer deaths, but it’s also one of the most preventable. Routine screening starting at age 45 — or earlier for those with risk factors — can detect precancerous polyps before they become cancerous.
Options for screening include:
- Colonoscopy: The gold standard for detecting and removing polyps.
- Fecal immunochemical test (FIT): Detects hidden blood in the stool.
- Stool DNA tests: Identifies genetic changes linked to cancer cells.
Rectal cancer symptoms can be easy to overlook, especially in the early stages when treatment is most effective. Paying attention to warning signs like rectal bleeding, changes in bowel habits, and unexplained weight loss can lead to earlier diagnosis and better outcomes.
If you notice any persistent gastrointestinal changes, don’t hesitate to speak with your doctor. With timely colorectal cancer screening, advanced treatments, and healthy lifestyle habits, rectal cancer can often be detected early and treated successfully.